In First, Aging Stopped in Humans: TAU Co-Study
New research finds that high pressure treatments can reverse two processes associated with aging and its illnesses
A first-of-its-kind clinical trial in human subjects: A new study from Tel Aviv University and the Shamir Medical Center indicates that HBOT (treatments with high-pressure oxygen) in healthy aging adults can stop the aging of blood cells.
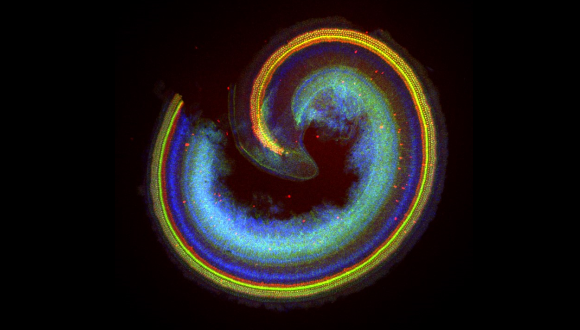
The researchers found that a unique protocol of treatments in a pressure chamber can reverse two major processes associated with aging and its illnesses: the shortening of telomeres – – protective regions located at both ends of every chromosome (the chromosomes contain the genetic material in the cell’s nucleus), and the accumulation of senescent (old and malfunctioning) cells in the body. Focusing on immune cells containing DNA, obtained from the participants’ blood, the study discovered a significant lengthening – up to 38% – of the telomeres, as well as a decrease of up to 37% in the presence of senescent cells.
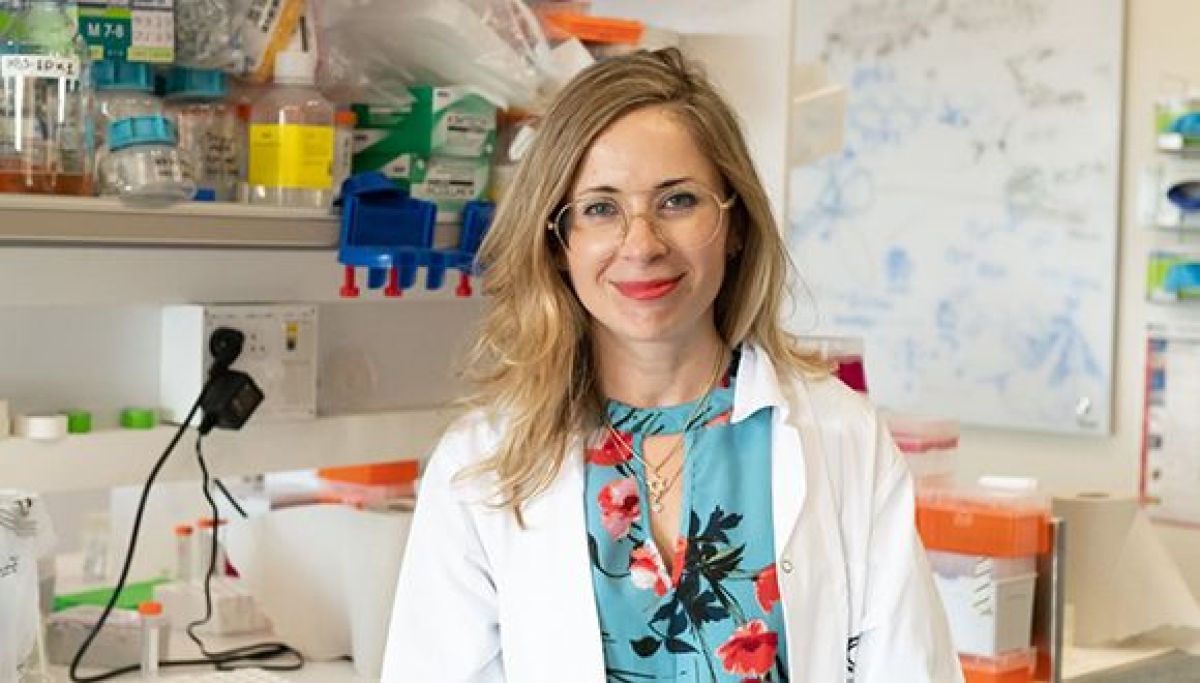
The study was led by Prof. Shai Efrati, faculty member of the Sackler School of Medicine and the Sagol School of Neuroscience at Tel Aviv University and Founder and Director of the Sagol Center of Hyperbaric Medicine at the Shamir Medical Center, and Dr. Amir Hadanny, Chief Medical Research Officer of the Sagol Center for Hyperbaric Medicine and Research at the Shamir Medical Center. The clinical trial was conducted as part of a comprehensive Israeli research program that targets aging as a reversible disease. The paper was published in the scientific journal Aging in November 2020.
Prof. Efrati explains: “For many years our team has been engaged in hyperbaric research and therapy – treatments based on protocols of exposure to high-pressure oxygen at various concentrations inside a pressure chamber. Our achievements over the years included the improvement of brain functions damaged by age, stroke or brain injury. In the current study we wished to examine the impact of HBOT on healthy and independent aging adults, and to discover whether such treatments can slow down, stop or even reverse the normal aging process at the cellular level.”
The researchers exposed 35 healthy individuals aged 64 or over to a series of 60 hyperbaric sessions over a period of 90 days. Each participant provided blood samples at four different points in time – before, during, at the end and after the series of treatments, and the researchers analyzed various immune cells (cells containing DNA) in the blood and compared the results.
The findings indicated that the treatments actually reversed the aging process in two of its major aspects: The telomeres at the ends of the chromosomes grew longer instead of shorter, at a rate of 20%-38% for the different cell types; and the percentage of senescent cells in the overall cell population was reduced significantly – by 11%-37% depending on cell type.
Prof. Efrati: “Today telomere shortening is considered the ‘Holy Grail’ of the biology of aging. Researchers around the world are trying to develop pharmacological and environmental interventions that enable telomere elongation. Our HBOT protocol was able to achieve this, proving that the aging process can in fact be reversed at the basic cellular-molecular level.”
Dr. Hadanny: “Until now, interventions such as lifestyle modifications and intense exercise were shown to have some inhibiting effect on telomere shortening. But in our study, only three months of HBOT were able to elongate telomeres at rates far beyond any currently available interventions or lifestyle modifications. With this pioneering study, we have opened a door for further research on the cellular impact of HBOT and its potential for reversing the aging process.”