Can Stem Cells Restore Bone Marrow?
Doubling adult stem cells for bone marrow and immune system regeneration.
An international research team, led by scientists from Tel Aviv University and Sheba Medical Center, has unveiled an innovative method for activating adult stem cells from human bone marrow, enabling their expansion outside the body for use in bone marrow regeneration and the construction of a new blood and immune system.
The findings, published in the prestigious journal Nature Immunology, represent a breakthrough that could significantly improve transplant success rates for patients who have undergone intensive chemotherapy, suffer from genetic disorders, or require a bone marrow transplant but are unable to source a sufficient number of stem cells from a donor.
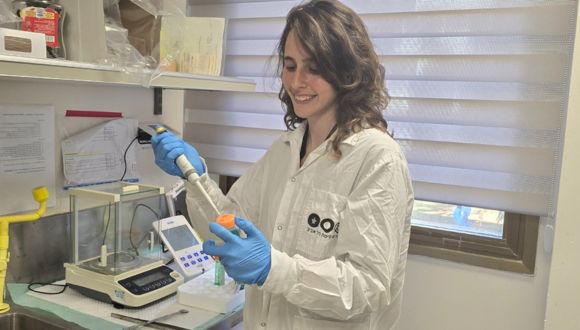
The study was led by Dr. Tomer Itkin from the Faculty of Medical and Health Sciences and the Sagol Center for Regenerative Medicine at Tel Aviv University, and the Neufeld Cardiac Research Institute at Sheba Medical Center, Tel Hashomer. The research also included contributions from leading medical institutions worldwide, including Weill Cornell Medical College and Hospital in New York, the Memorial Sloan Kettering Cancer Center (MSKCC), Mount Sinai Hospital, the University of Toronto Medical Center, and the Fred Hutchinson Cancer Research Center in Seattle.

Dr. Tomer Itkin.
Switching On Stem Cells
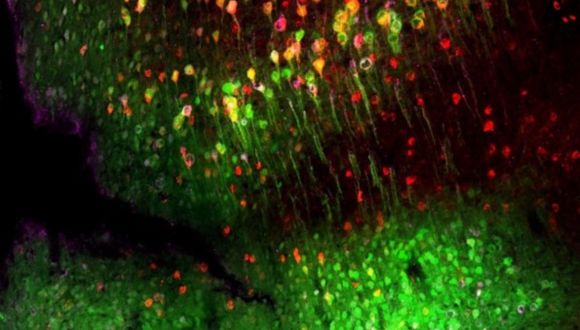
In the study, which is based on a comprehensive big data analysis of RNA sequencing and epigenetic DNA sequencing, the researchers identified a key protein—the Fli-1 transcription factor—that activates stem cells of the immune and blood system. These stem cells are highly active when sourced from umbilical cord blood but remain in a “dormant” and inactive state when obtained from adult bone marrow donors. Using modified mRNA technology—the same technology used to develop COVID-19 vaccines—the researchers successfully “awakened” the adult stem cells, allowing them to divide in a controlled manner without cancer risk. The activated cells were expanded on endothelial cells, which mimic the blood vessels that support stem cells in the bone marrow environment, demonstrating an enhanced ability to integrate and restore blood production under transplant conditions.
According to Dr. Itkin, “This new method significantly expands the available pool of stem cells for transplantation without relying on rare bone marrow donors. Additionally, the method can be used to treat patients whose stem cells have undergone genetic correction, such as those with thalassemia and hereditary anemia, as well as patients who have undergone multiple rounds of chemotherapy and have an insufficient number of stem cells for autologous transplantation“.
The key takeaway from the study is that activating stem cells through molecular programming, rather than arbitrary cell transplantation, substantially improves the success rates of regenerative treatments. The next stage of research involves testing the method in clinical trials to bring this groundbreaking technology into widespread therapeutic use. Furthermore, the researchers plan to apply the same therapeutic approach to regenerate additional tissues, including those without existing adult stem cells, such as the heart.