Whoops and cheers rip through the room as industrial engineering student Merav David looks on with amusement. She has just told 60 teenage girls on a tour of TAU’s Iby and Aladar Fleischman Faculty of Engineering that women are by far the highest achievers among the students in her third-year class. The girls on the tour study advanced math and science in Bat Yam high schools – defying the gender gap in science, technology, engineering and mathematics (STEM). This gap is evident from an early age and carries through university, where women represent fewer than 25% of STEM graduates in developed countries worldwide, even as they outnumber men in study programs overall. Starting young is critical according to Prof. Rachel Gali Cinamon, Head of TAU’s Jaime and Joan Constantiner School of Education: “The current system misses out on girls. We must engage them before they are tracked into non-STEM fields.”
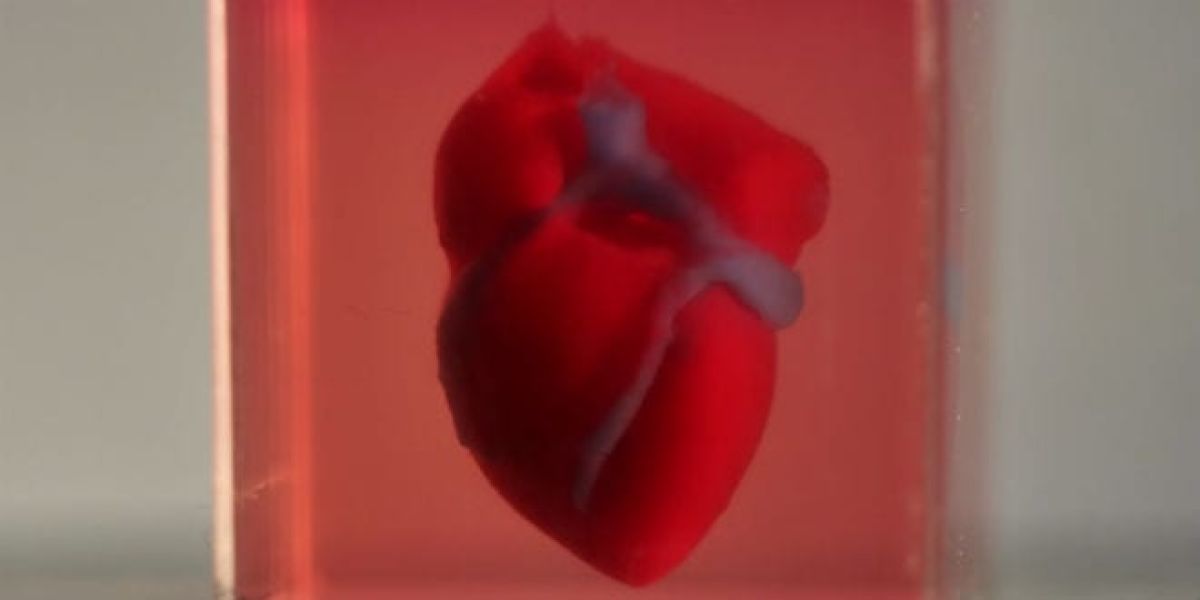
A new TAU program, “Girls Think Science,” is designed to spark girls’ interest in STEM subjects during the golden window of learning from 3rd to 6th grade. Girls from Israel’s social and geographic periphery, including Arabs and Orthodox Jews, enjoy experiential learning at STEM labs, guided by female students and researchers. The program expands upon engineering tours that Dr. Dana Ashkenazi of the School of Mechanical Engineering has been organizing on a volunteer basis for the past decade at TAU’s Engineering Faculty. Girls attending the tours get answers to questions such as “why is the sky blue?” at Prof. Avishay Eyal’s Optics & Photonics Lab, guided by doctoral student Lihi Shiloh; see the inner workings of the body with 3D printing of biological organs at Dr. Orna Sharabani-Yosef’s Tissue Engineering Lab; and encounter artificial intelligence (AI) robots at Dr. Goren Gordon’s Curiosity Lab.
During her PhD studies in the 1990s, Dr. Ashkenazi was the lone woman in a class of 40. This experience motivated her to introduce girls to the joys of science in the hope of recruiting more women to STEM. “My parents exposed me to scientific and engineering topics from a young age. But still, as a mother, I could see my daughters being steered toward humanities tracks at school. I tell them they can do whatever they set their minds to, but society says something else. Girls begin to question themselves, their abilities and their chances to succeed.”
Questioning one’s ability to succeed influences the high rate of attrition that increases with each higher education milestone among women in STEM. Prof. Cinamon, in conjunction with Israel’s Ministry of Science & Technology, studied this phenomenon and developed unique interventions for all stages of academic development, from BSc through post-doc. Interventions range from mentorship to reframing the post-doc as a unique family experience. “Among undergrads, MScs, and PhDs we found that academic identity – rather than academic achievement – is the major factor deter-mining whether a student will pursue higher level STEM studies. Women may have phenomenal grades and academic achievements, yet still may believe they are not good enough.”
The post-doc hurdle
But what are women’s chances of making it in STEM? The TAU President’s Advisor on Gender Equity Prof. Ilana Eli runs the numbers: “Women represent 54% of PhD candidates at TAU, but less than 50% of TAU lecturers and only 22% of professors. In STEM fields these percentages drop precipitously, with some departments employing only one female faculty member among nearly 50 men.
“These numbers reflect the past – professors today began their careers more than two decades ago. Yet these numbers also influence the future – our female students lack role models showing the academic path as accessible to women, especially in STEM,” says Eli. The postdoc is the most formidable obstacle for Israeli women in academia. By the time they complete their PhDs many are starting a family and a postdoc placement of two to four years abroad can seem untenable. TAU is now helping by awarding yearly stipends of $25,000 each for women postdocs in STEM.
“We grant five stipends annually. But deserving candidates are double that number and we wish we could grant more,” says Prof. Eli.
Other programs include a joint post doc in which women conduct research abroad under the auspices of a foreign university as well as at TAU, thus cutting the need for a multiyear relocation. The President’s office also sponsors stipends for travel with a nursing baby and caregiver, enabling new mothers to participate in international conferences essential for establishing themselves in academia.
Changing reality
TAU scientists are eager to boost the number of female faculty through Girls Think Science. “It’s simple math: The larger the pool of girls exposed to STEM, the greater the chance of women choosing to go into STEM fields, both in industry and academia,” says Prof. Shiri Artstein-Avidan, the only female full professor of pure math among over 40 professors at the Raymond and Beverly Sackler School of Mathematical Sciences and a 2016 Kadar Family Award winner. “My father is a mathematician. I want to bring girls who were not brought up in a scientific milieu to this fascinating world.”
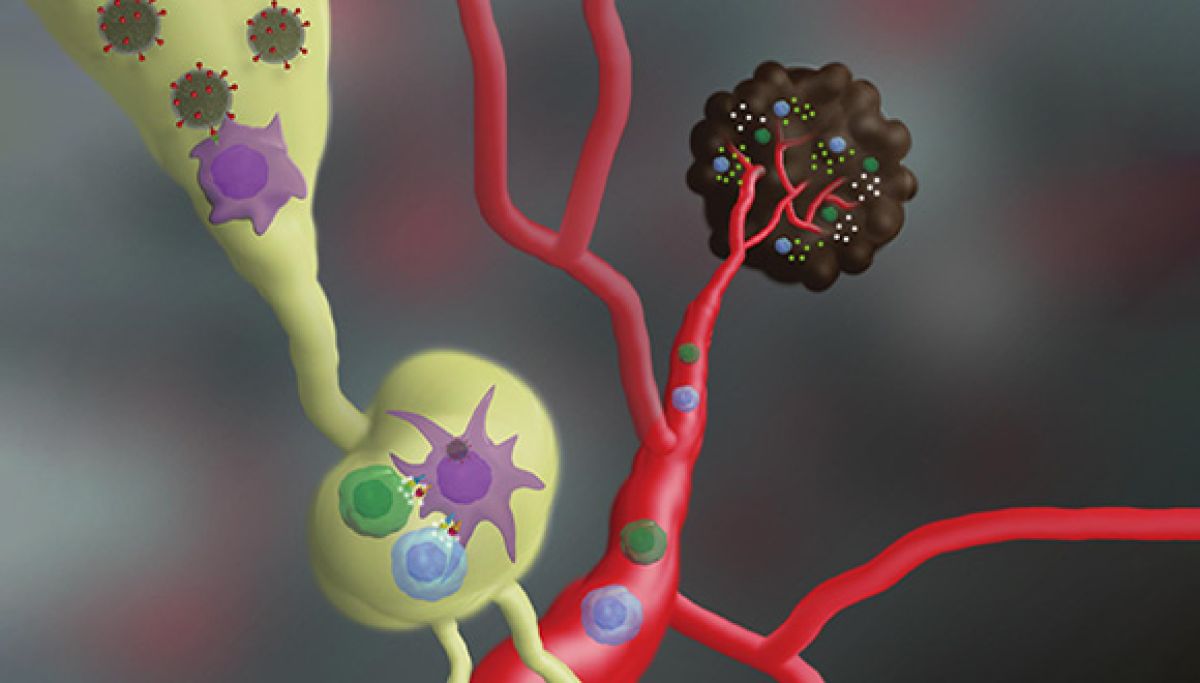
Dr. Vered Padler-Karavani of the George S. Wise Faculty of Life Sciences did not enjoy access to science in her home or local school. She grew up in a development town and discovered science through TAU’s long-running Dov Lautman Unit for Science Oriented Youth (now Youth University). “Starting early is important, as is having someone to look up to,” says Padler-Karavani. That is why she volunteers as Chair of ISEF—the Israeli Scholarship Education Foundation—which seeks to expand STEM among youth in Israel’s periphery. She is eager to host Girls Think Science participants in her lab where she studies how to target diseased cells through their protein and sugar coatings.
Role models are crucial, maintains Dr. Ashkenazi. “We hold our tours in the presence of female faculty members and students as mentors.” Ashkenazi believes that the program must engage students from Israel’s periphery, not just from the urban, affluent areas of central Israel because, “When it comes to these subjects, just being a girl places you in the periphery.”
Featured image: High school girls from Bat Yam touring the teaching laboratory at the Department of Materials Science and Engineering at the Iby and Aladar Fleischman Faculty of Engineering
 Prof. Berman, of TAU’s George S. Wise Faculty of Life Sciences, is being recognized for her outstanding achievements in the study of the growth and evolution of yeast. Prof. Berman, a Fellow of the American Association for the Advancement of Science (AAAS) and the American Society for Microbiology, uses yeasts, especially pathogenic yeasts, to address basic mechanisms of genome change that underlie rapid phenotypic responses to stress.
Prof. Berman, of TAU’s George S. Wise Faculty of Life Sciences, is being recognized for her outstanding achievements in the study of the growth and evolution of yeast. Prof. Berman, a Fellow of the American Association for the Advancement of Science (AAAS) and the American Society for Microbiology, uses yeasts, especially pathogenic yeasts, to address basic mechanisms of genome change that underlie rapid phenotypic responses to stress. 


 “We asked ourselves what fat cells were doing there and began to investigate,” adds Prof. Levy. “We placed the fat cells on a petri dish near melanoma cells and followed the interactions between them.”
“We asked ourselves what fat cells were doing there and began to investigate,” adds Prof. Levy. “We placed the fat cells on a petri dish near melanoma cells and followed the interactions between them.”