Is This the Future of Burn Care?
TAU researchers and Sheba Medical Center developed bioengineered skin that accelerates healing time.
Researchers from Tel Aviv University and Sheba Tel Hashomer Medical Center have developed an innovative bioengineered skin equivalent for grafting in burn victims. The bioengineered skin produced from the patient’s cells is more stable, robust, and flexible than current treatments, making it easier to handle. A full-thickness wound model, it achieved wound closure in half the time of standard therapies. This pioneering study was driven by the ongoing war and the surge in severe burn injuries, which underscored the urgent need for better treatment solutions.
The groundbreaking study was led by Prof. Lihi Adler-Abramovich and PhD student Dana Cohen-Gerassi from the Laboratory for Bio-Inspired Materials and Nanotechnology at the Goldschleger School of Dental Medicine, at TAU’s Gray Faculty of Medical and Health Sciences, in collaboration with: Dr. Ayelet Di Segni, Director of the Sheba Tissue Bank and the Green Skin Engineering Laboratory at Sheba; Dr. Amit Sitt from TAU’s School of Chemistry, Faculty of Exact Sciences, Prof. Josef Haik, Head of the Plastic Surgery Division and National Burn Center at Sheba; Dr. Moti Harats, Head of the Israeli National Intensive Care Burn Center at Sheba; Dr. Marina Ben-Shoshan and Dr. Adi Liiani scientists from the Green Skin Engineering Laboratory at Sheba; Prof. Itzhak Binderman from TAU’s Goldschleger School of Dental Medicine and Prof. Yosi Shacham-Diamand from TAU’s Fleischman Faculty of Engineering, as well as PhD candidate Tomer Reuveni and Offir Loboda from TAU. The paper was published in the prestigious scientific journal Advanced Functional Materials.

The research team from Tel Aviv University and Sheba Medical Center (From left to right): Dr. Amit Sitt, Dr. Marina Ben-Shoshan, Dr. Ayelet Di Segni, Prof. Lihi Adler-Abramovich & Dana Cohen-Gerassi.
“Surgical intervention is often essential for second-degree burns and above to restore skin, prevent infection, and save lives,” explains Prof. Lihi Adler-Abramovich. “The current gold-standard treatment is ‘autologous skin grafting’, in which healthy skin is harvested from another area of the patient’s body and transplanted onto the burn site. However, this approach has significant disadvantages, particularly the need to damage healthy tissue to treat the injury. This becomes especially problematic in cases of extensive burns, where the availability of intact skin is limited.”
Smart Skin That Heals You Faster
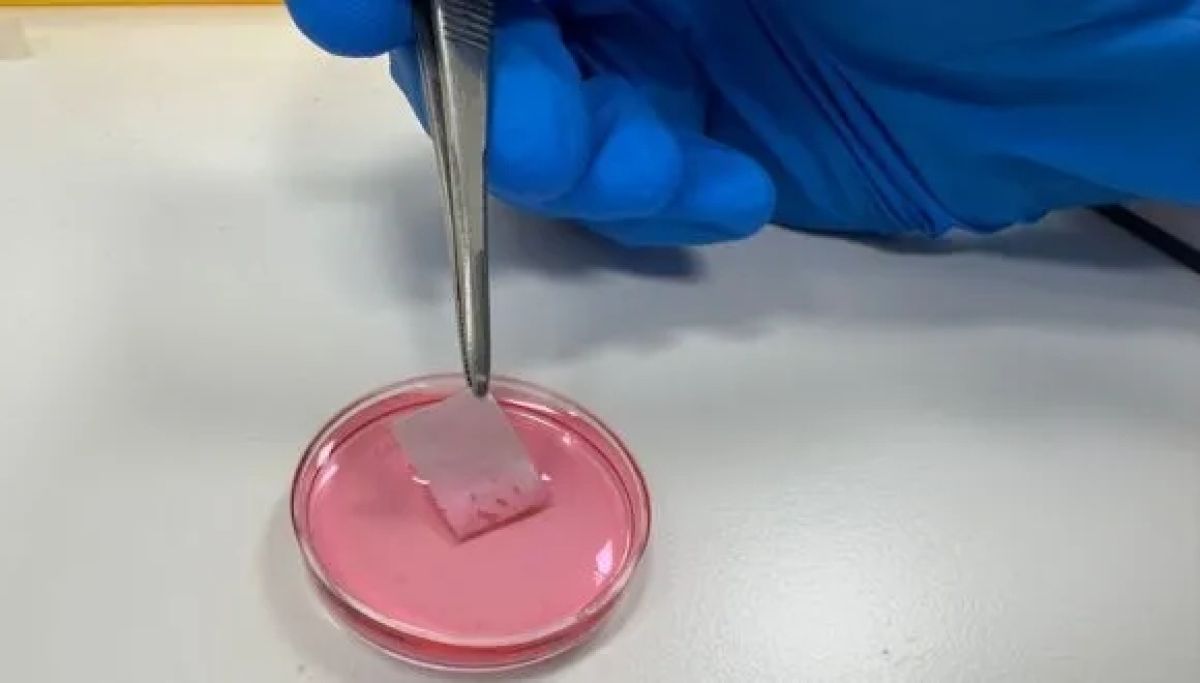
“One of the most advanced alternatives, currently offered in Israel only at Sheba Medical Center, is ‘cultured epidermal autograft’ (CEA). Instead of removing a large skin section, a small biopsy is taken, and cells extracted from that sample are cultured in the lab to produce skin grafts for transplantation. While this method avoids donor-site damage, it comes with several challenges: First, the skin cells are grown on a layer of mouse-derived feeder cells, requiring strict regulation to ensure no mouse cells remain in the graft; Second, once removed from the culture dish, the CEA shrinks by over 50%, significantly reducing yield up to 30 grafts may be needed to cover a single area, such as an arm or leg. Finally, the lab-grown skin consists of only the upper epidermal layer, making it extremely thin, fragile, and prone to curling at the edges.”
The need for advanced solutions is particularly urgent in wartime, with many soldiers suffering from burns. For both soldiers and civilians, a durable bioengineered graft could significantly improve chances for recovery and a good quality of life. “Since October 2023, Sheba has treated many young people with burn injuries,” says Dr. Ayelet Di Segni. “At such a time, bringing knowledge accumulated in the lab directly to the patient’s bedside becomes an urgent and tangible goal. We aim to develop a graft that can truly transform the process of recovery.”
Made from Your Own Cells
To address this challenge, researchers from Tel Aviv University and Sheba Medical Center collaborated to develop multi-cellular, multi-layered bioengineered skin grafts designed to mimic the properties and function of natural skin, without shrinking, tearing upon contact, or relying on animal-derived additives.
“We designed a nanofiber scaffold made of a polymer called PCL, which is already FDA-approved, and combined it with a bioactive peptide – a short amino acid sequence that promotes cell adhesion, growth, and proliferation,” explains PhD student Dana Cohen-Gerassi. “We then seeded this scaffold with skin cells derived from a patient’s biopsy. Remarkably, the cells organized themselves naturally: fibroblasts populated one side of the scaffold, while keratinocytes grew on the other – mimicking the structure of real human skin.”
Dr. Marina Ben-Shoshan, senior researcher at Sheba’s Green Center for Skin Graft Engineering, adds: “Our graft is unique in that it does not shrink, and is durable, flexible, and easy to handle. Implantation in model animals has yielded impressive results, accelerating the healing process. While the standard treatment closes half of the burn wound in eight days, with our method, this took only four days. Moreover, we observed that essential skin structures, such as hair follicles, began to grow.”
Dr. Amit Sitt from TAU’s School of Chemistry adds: “The nanofiber scaffolds are made from easily available biocompatible materials and produced via a scalable spinning process. In the future, this will enable large-scale production of fiber sheets, as well as incorporation of additional substances to facilitate the healing process.”
Prof. Yossi Haik of Sheba Medical Center concludes: “The bioengineered skin we’ve developed represents a true breakthrough in burn care. Made entirely from the patient’s cells, it is strong, flexible, easy to handle, and significantly accelerates healing. This is a major step towards personalized therapies that can greatly improve the recovery and quality of life of severe burn victims, both soldiers and civilians. In the next phase, we plan to conduct trials in additional models and advance the necessary regulatory processes to bring this innovative technology closer to clinical application.”